Now, we totally get that the words Membranous dysmenorrhea look more than a little intimidating. That’s because they totally are, and when you find out what they’re describing, you’ll get why. Full disclosure here, gang, this condition, also known as Decidual cast, or even Endometrial cast, could be considered a little on the graphic side. So what the actual what are we talking about? Let’s dive in…
What on Earth are we talking about?
The name Membranous dysmenorrhea, is until very recently, something that lots of us at Hormona towers had never heard before. And it’s thanks to our amazing community that it’s been brought to our attention — shout out the Hormona app and the incredible discussions that go on there.
One of our users had recently experienced this phenomenon and reached out to our medical experts for advice and reassurance. Which they got — our medical team seriously rocks. But that’s when we non-medical types realized that it was time we shine a light on this extremely rare, if extremely disconcerting, condition, just in case you ever need this knowledge.
So, let’s start at the very beginning.
Membranous dysmenorrhea: The what and when
If you’re someone who has, or ever had, periods, you’ll likely be aware that they involve the sloughing off and excretion of your endometrium, or uterine lining. That generally happens over the course of 2 to 7 days every month and can be accompanied by cramps, clots, and varying degrees of bloody discharge.
The eagle-eyed among you may well have spotted — no pun intended — the use of dysmenorrhea here. And there’s a good chance that you’re already aware that dysmenorrhea means painful periods, as lots of us experience that pain during our reproductive lives.
And yes, pain is definitely a feature of Membranous dysmenorrhea, as it can be excruciatingly painful. Thankfully, that pain is, generally, temporary and often disappears completely once the event is over. The event? Well, that’s, gulp, passing your endometrium, WHOLE, through a cervix that’s not dilated, with no pain relief and, probably, no idea what the actual what is happening to you.
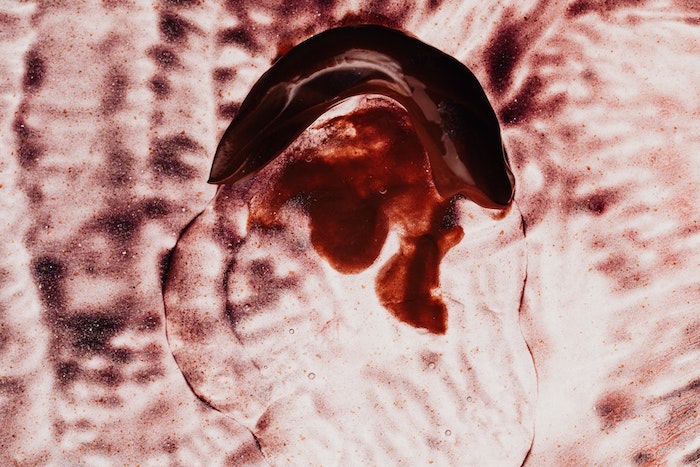
It’s been compared to placental delivery after giving birth, and to be honest, that’s a pretty good description. Because the result of this event is tissue around the size and shape of the inside of your uterus leaving your body. In essence, if you’re ever unlucky enough to experience this event, you’ll see what most of us never see — your actual endometrium. In its entirety. As opposed to little bits at a time.
But, and this bit is super-important gang, this event is incredibly rare. We’re not talking heavy periods, large clots, or painful cramps, as bad as they are. If this has happened to you, you’ll definitely know it. And if it does, please, please tell your healthcare team as soon as possible.
Membranous dysmenorrhea: The how and why
Given that this is a rare condition that only affects those of us with periods and uteruses, there’s almost no research or real explanation of the how or the why. Even though medicine has known about it since the 18th century…
Here’s what we do know. Membranous dysmenorrhea, Decidual cast, or Endometrial cast — however you’re comfortable describing it — generally occurs between the ages of 20 and 40. And we say generally because we’ve seen a case study where this exact thing happened to a 10-year-old girl. Who must have been terrified.
Now, the good news: For most, it’s a one-time-only occurrence. Except, that is, for our user, who’s experienced it every month, for at least a year.
And as far as medicine is able to tell, Membranous dysmenorrhea may well have a few causes, although no one is sure which is correct. Chances are they’re all a little bit right, depending on the case:
- Ectopic pregnancy, where a fertilized egg grows outside of the uterus
- Endometrial infection or dead tissue
- Hormonal contraceptives containing synthetic progesterone
If you’re a regular Hormona, you’ll be well aware that where anything even remotely hormonal is concerned, chances are that causes will be individual to the patient. So there may well be other things at play here that we just don’t know about. But because the event is so rare, it’s unlikely we’ll get a definitive answer any time soon.
Our medical team answers your questions
Now, this is a bit of an unusual situation for us, as it’s rare that we haven’t heard of uterine-related events and conditions. So we thought we’d bring our medical team on board for this part. Ladies, meet Dr Anna Targonsyaka, one of our most talented and active doctors. She’s here to answer the most popular questions around this topic, and educate us all.
But if we haven’t covered something you want to know, please reach out and tell us. Likewise, if this is something you’re currently living with — we’ve got to get this knowledge out to as many women as possible.
Dr. Anna, it’s over to you…
Hey Anna! Thank you so much for talking to us! So, are painful periods or large clots signs of Membranous dysmenorrhea?
My super short answer is yes and no. The reason for that is, that although painful periods and large clots are signs of membranous dysmenorrhea, they aren’t specific signs. The single most noticeable sign of this condition is the passage of whole or nearly whole pieces of the inner uterine lining during the first or second day of the period, which looks like an upside-down triangle and can be exceptionally painful. Therefore, the presence of large clots alone does not indicate this condition.
How common is Membranous dysmenorrhea?
Nobody knows the real prevalence of this condition. So, currently, it’s considered rare. But we think it was first described by Giovanni Battista Morgagni in the 18th century, which means we’ve known about it for a while.
There are reported cases from different parts of the world, which amount to less than 1% if converted to numbers. However, due to underreporting, the true prevalence may actually be higher.
How might hormonal birth control contribute?
So, there is no evidence that hormonal contraceptives cause Membranous dysmenorrhea, and no need to label this condition as a rare side effect of using them. Therefore, please don’t stop using your medication after reading this!
Based on the medical history in the reported cases of this condition, its development can be associated with synthetic progesterone, irrespective of the form of hormonal contraception used — whether it’s oral contraceptives, injectable progesterone, or an implantable progesterone delivery system.
As most cases are related to adolescence, there is a possibility that the uterus responds unexpectedly to the high doses of synthetic progesterone administered for some reason, leading to abnormal growth, and then shedding, of its inner lining.
Does it affect fertility in any way?
No, Membranous dysmenorrhea doesn’t affect fertility. Or, at least there are no reported cases of that happening.
What should I do if it happens to me?
First of all, please don’t panic. Schedule an appointment with your healthcare provider, such as a gynecologist or primary care physician, to discuss your symptoms and concerns. And be prepared to provide detailed information about your menstrual cycle, symptoms, and any treatments you’ve tried. This information can help your healthcare provider make an accurate diagnosis.
Then, based on your evaluation, your healthcare provider may recommend specific treatments or management strategies to address your symptoms. Typically, this will include pain relief measures.
Finally, keep track of your symptoms. This information can help you and your healthcare provider assess the effectiveness of any treatments and make adjustments as needed. And, I just want to reiterate that Membranous dysmenorrhea is extremely rare, so chances are you’ll never experience it. That said, knowledge is power, so make sure you tell all the women you know what you’ve learned!
Membranous dysmenorrhea: TLDR
More than period pain and clots, Membranous dysmenorrhea involves passing your endometrium whole, in its entirety, in one go. It’s painful, and, let’s be honest, a bit of shock. But it’s also, in lots of cases, a one-off event related to synthetic progesterone, an infection, or an ectopic pregnancy.
Once you’ve passed the endometrium, the pain should recede, and your periods should resume in their usual way during your next cycle. And aside from the traumatic memories, your physical wellbeing will hopefully be unaffected. Uteruses are amazing, and can take care of themselves in ways we’re still learning about.
That said, if you experience Membranous dysmenorrhea, please tell someone. Because the more women who come forward, the more we’ll know, and the more women we can educate and help when it happens to them. We’ve got to look after each other, gang, at least until medicine catches up with our uteruses.